Contraceptives
WSS interviewed three anonymous student sources for this article. Anonymity is used to protect the privacy of students commenting on contraceptives. View the editorial policy at wsspaper.com.
From a young age, kids are taught preventative measures against the cold or flu: vaccines, masks, washing hands and coughing into the elbow. However, these aren’t the only health concerns that young people need awareness of. Contraception, a frequently disregarded and shamed topic, has many stigmas surrounding the usage of types of birth control. Feelings of embarrassment regarding contraception can hinder necessary conversations, leading to misconceptions arising.
However, contraception is a topic that impacts a large percentage of the population, with over 65% of women aged 15-49 using some form of birth control. Dr. Michael Colburn, Head of Adolescent Medicine at the University of Iowa, believes the definition of contraception can differ depending on the person.
“I believe contraception is everything and anything that leads to people being in control of when they are ready to be parents,” Colburn said.
Colburn advocates for care that allows patients to choose individualized plans for contraceptive use.
“Our statement [at the University of Iowa Hospitals and Clinics] is that you have the ability to consent and choose treatment in certain realms,” Colburn said.
In line with the University’s commitment to providing accessible treatment, the University of Iowa’s Adolescent Clinic encounters many teens who take control of obtaining their own contraceptive options.
“The vast majority of people [coming to the clinic for contraception] are the patients themselves,” Colburn said. “In this clinic, we’re really helping them be goal-focused. Asking, ‘Why are you here? What’s going on?’ and as part of routine care, we talk about sexual health.”
Studies from the National Institutes of Health have concluded that when healthcare providers initiate sexual health discussions, adolescents are more likely to get tested for sexually transmitted illnesses (STIs). Human Papillomavirus (HPV) and Human immunodeficiency Virus (HIV) are among many examples of STIs. HPV is the most common STI in the United States, with a majority of infections among teens and young adults. Although teens can make many health-related decisions independently, Colburn points out some exceptions.
“In this state, you can consent to sexual health preventative stuff; you can get your HPV shot without your parent’s consent, you can do screenings, you can get all your sexual health testing and you can get treatment,” Colburn said. “The only time [it] gets a little weird is if you are getting tested for HIV and your HIV [test] is positive. In Iowa, I have to report that to a caregiver.”
In 27 states, including Iowa, all individuals are allowed to consent to contraceptive services at a specified minimum age, with Iowa’s being 12 years old. However, 19 states only allow some minors to consent to contraceptive services, such as people with a health issue or who are married or pregnant. Despite the limitations some teens face, Ashley Guerrero, the University of Iowa’s Clinical Coordinator for Adolescent Medicine, believes it’s essential to educate teens and their families about contraceptive use.
“It may not be appointment one or appointment two that we really get through to them, but our goal is to educate the patient,” Guerrero said. “Sometimes the family too, because maybe the patient’s on board, but the family isn’t. Just because we’re giving a kid birth control doesn’t mean we’re saying, ‘Hey, go out and have a bunch of sex.’”
Although this is often an uncomfortable subject for teens and their families, Colburn believes transparency is the best course of action when providing care.
“Young adults are going to lose so much faith in the system if we manipulate care for the parents’ benefit,” Colburn said. “We don’t want to trick parents, but we understand that sometimes you’re not ready to talk to your parents yet, so we might coach you on how to talk about why you have [contraceptives].”
However, Guerrero reminds teenagers that they are entitled to a private doctor’s visit without their parents in the room.
“Always remember that you’re open to having these conversations with your primary care provider,” Guerrero said. “Your parents should be leaving during the [doctor’s] visit anyway. That’s our standard of care.”
Colburn agrees, noting that guardians often have their own opinions about teens’ contraceptive use that may conflict with what the teen wants or needs for themself.
“I really think birth control is your [own] decision and not to help alleviate someone else’s fear,” Colburn said. “But it’s important that you can tell me what is actually going on so that we are able to make the best decisions for you.”
Nonetheless, Guerrero believes it is important to take precautions and be prepared if things don’t go as planned.
“We don’t know what your choices are going to be [beforehand], and when you’re in the heat of the moment, it’s not the time to think, ‘Oh, I should be on birth control,’” Guerrero said.
Additionally, Colburn reminds teens that there are many ways to obtain contraceptives if needed.
“If somebody’s like, ‘I want this, but I can’t get it,’ you can, because there are resources in the community. There are places here that will see uninsured people,” Colburn said.
An anonymous student source found the contraceptives that she needed were easily available.
“Both [the birth control pill and Nexplanon] have been very accessible; I was able to get my Nexplanon the day of. It was like a two-minute process,” the source said. “There weren’t as many barriers for me, but I know for IUDs, there was a pretty long waitlist, and a lot of people needed anesthesia for [IUD placement]. That probably would have been a bigger barrier if that was what I had chosen to do.”
Colburn suggests teens who are looking for birth control options should begin with non-hormonal contraceptives.
“I want your body to use your own hormones for a bit, because you still have about four centimeters of growth that can still happen height-wise after you have your first period, and if I put you on estrogen-containing birth control pills, that gets a little stunted,” Colburn said.
Despite providing safe preventative measures, contraceptives also come with side effects. When taking birth control pills to combat painful period cramps, an anonymous source said she experienced increased fatigue. However, despite these negative side effects, the source wanted to remain on birth control.
“I noticed I had a lot less energy,” she said. “But I chose to take [birth control] consistently, even if it was always a very crazy hormonal roller coaster.”
After transitioning to Nexplanon, a birth control implant, the same source said these exhaustion side effects, along with cramping, went away. However, she acknowledges her positive experience may not be replicable for every person.
“I will occasionally get cramps, but they’re still not as bad [as before any birth control],” the source said. “I haven’t really had any negative side effects with Nexplanon, but I know a lot of other people have, so it really just depends on the person.”
However, because Nexplanon has worked well for her, the source plans to continue using it.
“I’ve heard a lot of people have really difficult times finding birth control options that work for them like I did,” she said. “So [now that] I found this one, I’ll try to stick to it as long as I possibly can.”
Prior to going on hormonal birth control, one of the anonymous sources heard online about breakthrough bleeding, a symptom of hormonal birth control where a person will bleed between their regular period cycles.
“I heard some people bleed for six months straight, which was something I was really scared about,” she said. “I was like, ‘I can’t do this, my period cramps are already so bad.’”
Though some online conversations initiate apprehension about certain types of birth control, Colburn notes some may do the opposite and ignore negative side effects.
“Sometimes when people talk to you about [implants], they make it sound like it’s really good because it’s a really effective birth control,” Colburn said. “But you might not get the full picture of how random your bleeding can be after you get it, and that happens to a lot of people.”
Because of the variety of contraceptive options available, Colburn advocates searching for an individual’s best fit.
“You can stop [any contraceptive and its side effects],” Colburn said. “So if it’s not a good fit for you — even if you have a device in your uterus — it can come out. We say it lasts eight years, but it doesn’t have to stay in place for eight years.”
Though contraceptives are mainly associated with impeding pregnancy, a third of teens in the United States taking oral contraceptives use them exclusively for reasons besides pregnancy prevention. One of the leading motivations, with 14% of American women, is preventing acne. There are four birth control pills recommended for treating hormonal acne, which work by lowering testosterone levels and, in turn, lowering levels of oil and sebum, which can clog pores and cause pimples.
An anonymous source found that her birth control, contrary to her belief, worsened her acne.
“The [birth control] that I take is supposed to help with acne,” the anonymous source said. “It’s one that you take specifically for acne, but it did the opposite for me.”
Another anonymous source wanted to regulate her hormones due to painful symptoms and an irregular menstrual cycle.
“I’ve had a really heavy flow since I first got my period, and I was having really bad hormonal acne, so I just wanted to figure it out,” the anonymous source said.
However, birth control didn’t work for her due to concerns that arose after consulting her pediatrician.
“I asked my pediatrician about [hormonal birth control] and she originally agreed, but because I have a family history of blood clotting and strokes, we decided it was best not to [use hormonal birth control] because birth control put me at high risk. I was offered other [non-hormonal] alternatives, like an arm implant or an IUD, but I decided against it,” the source said.
Because of the combined risk of her family’s medical history and birth control’s side effects, this anonymous source decided to forgo contraceptive use and instead found other alternatives to her irregular menstruation cycle.
“I ended up going to the dermatologist for my acne, but my periods are the same, so it can be really frustrating; I’ve had to miss school because of the pain,” the source said.
Religious beliefs play a part in some people’s decision to go on birth control. Some religions, like Catholicism, don’t condone the use of birth control, while others permit its use in certain circumstances and specific forms. However, birth control is becoming an increasingly popular option for family planning amongst younger generations. With more transparency in using contraceptives, the number of women using a modern method increased from 663 million to 851 million between 2000 and 2020.
An anonymous source said she finds it easier to talk about contraceptives with people her own age.
“I have a lot of religious family, and I don’t ever mention [contraceptives] in front of them. I’m open with friends and in high school because I feel like everyone’s in the same boat,” she said. “I’d rather people know about something I’m having a good experience with because I’ve seen so many of my friends have a really bad experience on the pill. I’d rather them know that you don’t have to be miserable on birth control.”
Even though there is more openness to contraception, many misconceptions about its effects remain prevalent. Colburn believes they impede teenagers’ ability to make fully informed decisions.
“These misconceptions that birth control is going to turn you into a rabid sexual beast are ridiculous,” Colburn said. “When you are ready to become a sexual person, you will become a sexual person. We need to make it less complicated for you because I want you to have safe and respectful relationships.”
An anonymous source believes online discussions can misconstrue how contraceptives will have varying effects on each individual.
“The biggest misunderstanding about contraceptives is that they’re all the same for you,” she said. “People say birth control pills suck, IUDs suck and everything birth control sucks, but it really depends on the person. I went into [my birth control appointment] very scared that I would have a bad experience, but I’m so glad I didn’t listen to the stigmas that I heard online.”
Another widespread misunderstanding regarding birth control is that it can affect a person’s fertility or ability to conceive later. However, research has shown this isn’t true. Colburn suggests this misconception can stem from other causes.
“No birth control causes infertility,” Colburn said. “What might happen is you use hormonal birth control, and then you didn’t use condoms because you were relying on your hormonal birth control, and then you started having sexually transmitted infections that led to scarring, and then infertility.”
However, if a person has concerns about the birth control or contraceptive device they’re utilizing, Colburn wants them to remember there are many alternatives available.
“[It’s important] to have honest conversations and know that you can stop any [contraceptive],” Colburn said. “I think we sometimes get worried that if we make a decision, we have to commit to it, but you guys will learn that you don’t. If it’s not a good fit for you, it’s not a good fit for you.”
Another common misconception Guerrero has encountered is that hormonal birth control inhibits the spread of STIs. Guerrero stresses that barrier protection, such as condoms or dental dams, should be used alongside hormonal contraceptives to prevent STIs. This is important, as not only do STIs cause extreme discomfort, but they can also lead to more serious consequences, such as cardiovascular diseases and infertility.
“Birth control doesn’t prevent STIs. You need to have a physical barrier to prevent STIs,” Guerrero said. “You can still get pregnant on birth control, and you’re not decreasing the risk of STIs at that point, so barrier protection is very important.”
Because of the impact that misconceptions can have on teenagers’ trust and use of contraceptives, Guerrero stresses the importance of discussion and education about birth control.
“This needs to be more of an open conversation with people,” Guerrero said. “I don’t know why there’s this stigma that we can’t talk about birth control. We’re all humans; the majority of us are going to have sex at some point in our lives.”
Your donation will support the student journalists of West High School. Your contribution will allow us to purchase Scholarship Yearbooks, newsroom equipment and cover our annual website hosting costs.
-
 Award winnersDigital footprints: AI’s environmental toll
Award winnersDigital footprints: AI’s environmental toll -
 Award winnersHow women’s wrestling found a home in Iowa City
Award winnersHow women’s wrestling found a home in Iowa City -
 Award winnersWhere excellence is a tradition, but where stress thrives
Award winnersWhere excellence is a tradition, but where stress thrives -
 Award winnersKindness, community and compliments
Award winnersKindness, community and compliments -
 Award winnersBurnt by the bell
Award winnersBurnt by the bell -
 Award winnersSubstantially limited
Award winnersSubstantially limited -
 Award winnersWest High's fragrance connoisseur: ScentedGent
Award winnersWest High's fragrance connoisseur: ScentedGent -
 Award winnersMusic on the mind
Award winnersMusic on the mind -
 Award winnersFlour Power by Finnley
Award winnersFlour Power by Finnley -
 Award winnersA new vision for elementary education
Award winnersA new vision for elementary education -
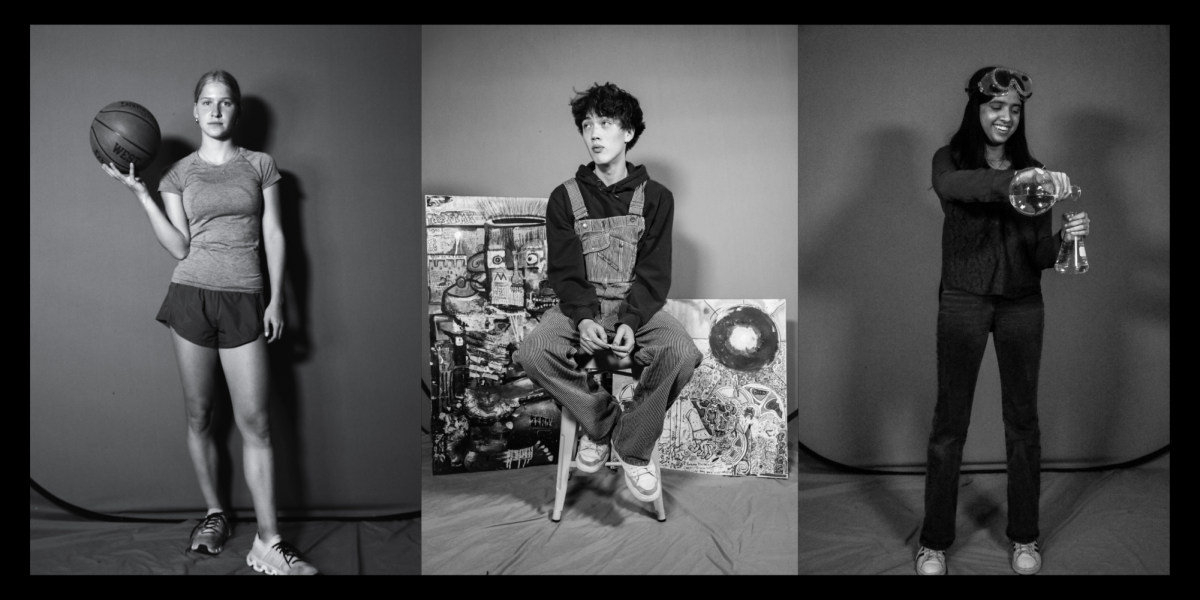 FeatureWSS 2025 People of the Year
FeatureWSS 2025 People of the Year -
 FeatureGone digital: the return of digital cameras
FeatureGone digital: the return of digital cameras -
 FeatureMiles for mental health
FeatureMiles for mental health -
 FeatureService and sacrifice
FeatureService and sacrifice -
 FeatureStitching sustainably
FeatureStitching sustainably -
 FeatureSenior futures
FeatureSenior futures -
 FeatureBrad Stiles: championship caliber coaching
FeatureBrad Stiles: championship caliber coaching -
 FeatureBack in time
FeatureBack in time -
 FeatureDriven, dangerous and distracted
FeatureDriven, dangerous and distracted -
 FeatureClass of 2025 senior columns
FeatureClass of 2025 senior columns -
 Health & ScienceBreaking the cycle
Health & ScienceBreaking the cycle -
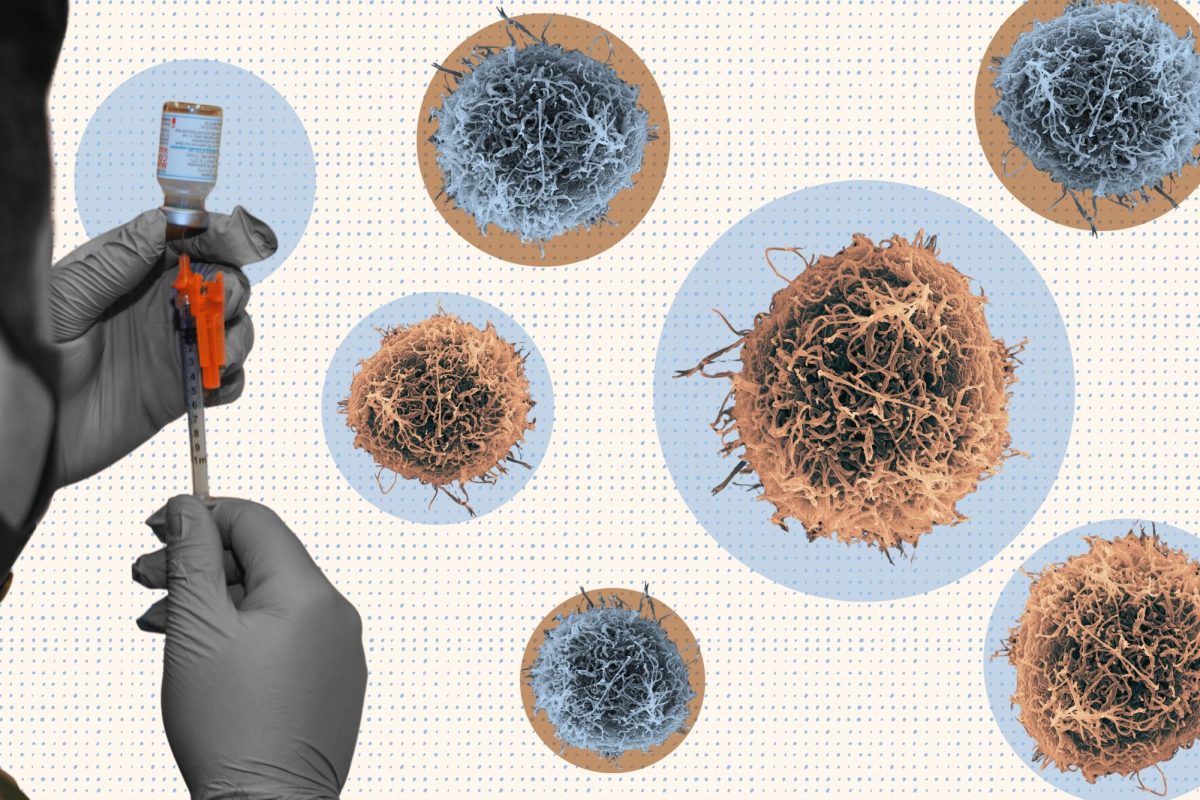 Health & ScienceThe vac-scene
Health & ScienceThe vac-scene -
 Health & ScienceRed Cross Club’s fifth blood drive brings in 50 units
Health & ScienceRed Cross Club’s fifth blood drive brings in 50 units -
 Health & ScienceWest High holds its first winter blood drive amidst a national blood shortage
Health & ScienceWest High holds its first winter blood drive amidst a national blood shortage -
 Health & ScienceFinding green in the gray area
Health & ScienceFinding green in the gray area -
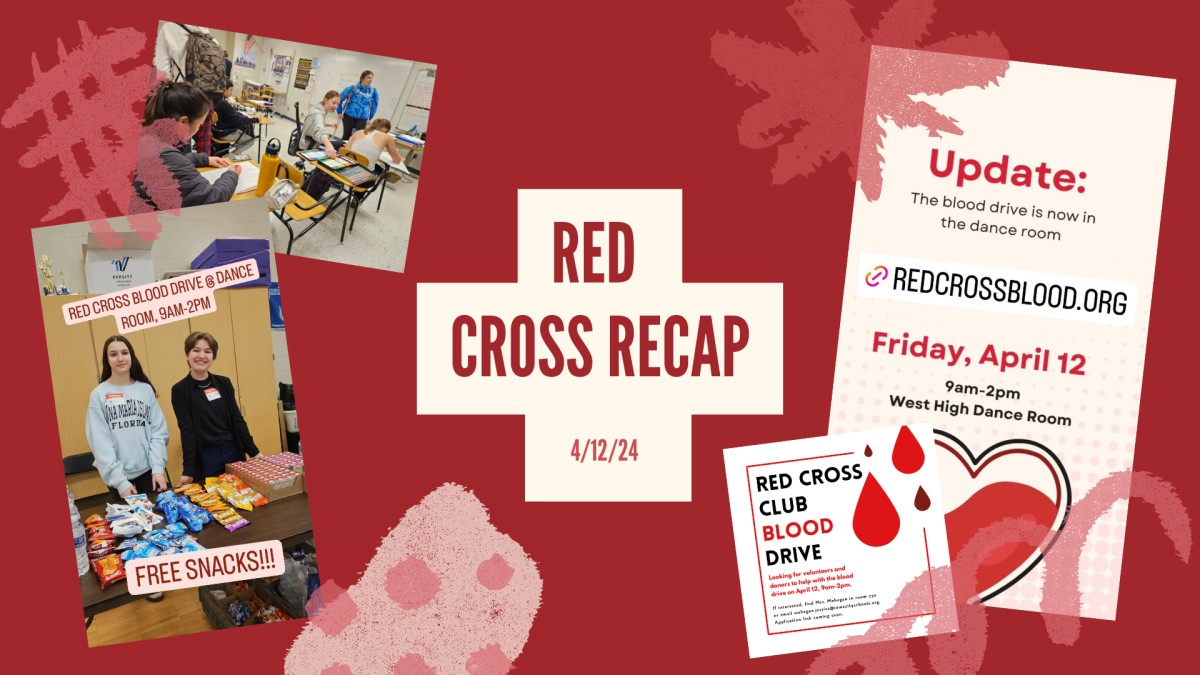 Health & ScienceRed Cross recap
Health & ScienceRed Cross recap -
 Health & SciencePowered up
Health & SciencePowered up -
 Health & ScienceBringing the spotlight effect into focus
Health & ScienceBringing the spotlight effect into focus -
 Health & Science1-2-3, eyes on me
Health & Science1-2-3, eyes on me -
 Health & ScienceMedicated
Health & ScienceMedicated